Development of Potential Harmful Foot Conditions From Wearing Flip Flops
 There are patients who have found their gait or walking style may have been altered if their lifestyle includes frequently wearing flip flops. The heel and ankles can negatively be affected, in addition to the skin on the feet when flip flops with no backs are worn often. Many people choose to wear this type of shoe for their ease and colorful designs, despite the potential damage they may cause. The toes can naturally scrunch in an effort to keep the shoe on the foot and performing this motion repeatedly can overstretch the plantar fascia, which is the band of tissue that connects the heel to the toes. If you enjoy wearing flip flops,please consult with a podiatrist who can recommend a more supportive sandal that can have less harmful side effects on the overall foot.
There are patients who have found their gait or walking style may have been altered if their lifestyle includes frequently wearing flip flops. The heel and ankles can negatively be affected, in addition to the skin on the feet when flip flops with no backs are worn often. Many people choose to wear this type of shoe for their ease and colorful designs, despite the potential damage they may cause. The toes can naturally scrunch in an effort to keep the shoe on the foot and performing this motion repeatedly can overstretch the plantar fascia, which is the band of tissue that connects the heel to the toes. If you enjoy wearing flip flops,please consult with a podiatrist who can recommend a more supportive sandal that can have less harmful side effects on the overall foot.
Flip-flops can cause a lot of problems for your feet. If you have any concerns about your feet or ankles, contact John Horlebein, DPM from Northern Cascades Foot & Ankle, LLC. Our doctor will assist you with all of your foot and ankle needs.
Flip-Flops and Feet
Flip-flops have managed to become a summer essential for a lot of people. While the shoes may be stylish and easy to slip on and off, they can be dangerous to those who wear them too often. These shoes might protect you from fungal infections such as athlete’s foot, but they can also give you foot pain and sprained ankles if you trip while wearing them.
When Are They Okay to Wear?
Flip-flops should only be worn for very short periods of time. They can help protect your feet in places that are crawling with fungi, such as gym locker rooms. Athlete’s foot and plantar warts are two common fungi that flip-flops may help protect your feet against.
Why Are They Bad for My Feet?
These shoes do not offer any arch support, so they are not ideal for everyday use. They also do not provide shock absorption or heel cushioning which can be problematic for your feet. Additionally, you may suffer from glass cuts, puncture wounds, and stubbed toes since they offer little protection for your feet.
More Reasons Why They Are Bad for Your Feet
- They Slow You Down
- May Cause Blisters and Calluses
- Expose Your Feet to Bacteria
If you have any questions, please feel free to contact our office located in Chelan, WA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Flipping Out About Flip Flops
Although it may be tempting to wear flip-flops in warm weather, they are not the best choice of footwear for your feet. Flip-flops may be ideal for the beach, pool, spa, and shared showers, but you should avoid wearing them unless it is completely necessary.
Flip-flops only have a small strip of fabric holding your foot in place, but your toes need a better grip to keep your foot in place. The repetitive gripping can lead to an overuse of your muscles, which could result in tendinitis. This is only one of the many problems that stem from wearing flip-flops too often.
Flip flops aren’t good for extensive walking because they fail to offer arch support, heel cushioning, or shock absorption. As a result, people who wear flip flops are at a higher risk of experiencing an ankle sprain. Additionally, these shoes offer little protection for your feet, putting those who wear them at a greater risk for stubbed toes, glass cuts, and puncture wounds.
Although flip flops aren’t recommended for everyday use by anyone, it is especially important for diabetics to avoid them. A diabetic foot injury can easily become very serious, and it may even lead to amputation.
If you are experiencing pain from wearing flip-flops, you shouldn’t be hesitant to replace them with a more comfortable shoe that offers more support. If your flip-flop foot pain doesn’t go away, you should seek assistance from a podiatrist right away. It is possible that you may have a more serious foot problem such as a stress fracture or arthritis.
Home Care for Cracked Heels
 When the feet become too dry, the skin on the heels can harden and crack. Cracked heels can be unsightly and uncomfortable. In some cases, the cracks can be deep, painful, and may even bleed. Treating and preventing dry, cracked heels begins with establishing a daily foot care routine. Soak the feet for at least 10 minutes in plain water and pat them dry, then gently rub your heels with a loofah to remove dead skin. Next, apply a thick moisturizer to the heels and put on cotton socks to seal in the moisture. If home treatments are not effective, it is suggested that you see a podiatrist for treatment.
When the feet become too dry, the skin on the heels can harden and crack. Cracked heels can be unsightly and uncomfortable. In some cases, the cracks can be deep, painful, and may even bleed. Treating and preventing dry, cracked heels begins with establishing a daily foot care routine. Soak the feet for at least 10 minutes in plain water and pat them dry, then gently rub your heels with a loofah to remove dead skin. Next, apply a thick moisturizer to the heels and put on cotton socks to seal in the moisture. If home treatments are not effective, it is suggested that you see a podiatrist for treatment.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact John Horlebein, DPM from Northern Cascades Foot & Ankle, LLC. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact our office located in Chelan, WA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels may make you want to think twice about showing off your feet in warmer weather. However, cracked heels may be harmful to more than just the appearance of your feet. If deep fissures and cracks develop in your heels, they may make walking and standing painful for you. Additionally, these openings make way for germs to enter through your skin and cause infection.
There are several different causes of cracked heels. One of the most common reasons for this ailment is dry skin. This problem may make your keeps feel rough tight and itchy. Dry skin may be caused by cold air, extremely hot water, harsh soaps, and aging. Skin disorders such as eczema and psoriasis may eventually lead to dry skin. In some cases, complications may arise from cracked heels. Some of these complications are a loss of feeling in the heel, cellulitis, or a diabetic foot ulcer.
There are ways you can try to prevent getting cracked heels. One of the best ways to do so is to avoid wearing flip flops and sandals because these shoes increase your risk of drying out your feet. You should also avoid wearing shoes with a tall skinny heel, because these shoes cause your heel to expand sideways. At night, you should slather on a thick moisturizing cream on your feet and then cover them in socks to keep your feet moisturized overnight. Drinking water to stay hydrated is also a good way to ensure that your skin doesn’t become dry.
If you suffer from a severe case of cracked feet, you should make an appointment with your podiatrist to see what treatment methods are best for you.
Treatment for Hammertoe
 Hammertoe is a type of foot deformity in which the toes bend upward at the middle joint, giving them a hammer-like appearance. This condition is usually caused by a muscle or tendon imbalance, but can be aggravated by wearing shoes that are too tight or narrow in the front or have excessively high heels. In the initial stages, the hammertoe may still be flexible and the toes can be straightened. In later stages, the toes can become rigid and you will not be able to straighten them. Flexible hammertoe can be treated by wearing shoes that are comfortable and have a wide toe box, wearing orthotic inserts, and stretching and exercising the toes. Rigid hammertoe may require surgery to correct it. If you have hammertoe, please consult with a podiatrist to see which treatment options may be right for you.
Hammertoe is a type of foot deformity in which the toes bend upward at the middle joint, giving them a hammer-like appearance. This condition is usually caused by a muscle or tendon imbalance, but can be aggravated by wearing shoes that are too tight or narrow in the front or have excessively high heels. In the initial stages, the hammertoe may still be flexible and the toes can be straightened. In later stages, the toes can become rigid and you will not be able to straighten them. Flexible hammertoe can be treated by wearing shoes that are comfortable and have a wide toe box, wearing orthotic inserts, and stretching and exercising the toes. Rigid hammertoe may require surgery to correct it. If you have hammertoe, please consult with a podiatrist to see which treatment options may be right for you.
Hammertoes can be a painful condition to live with. For more information, contact John Horlebein, DPM of Northern Cascades Foot & Ankle, LLC. Our doctor will answer any of your foot- and ankle-related questions.
Hammertoe
Hammertoe is a foot deformity that occurs due to an imbalance in the muscles, tendons, or ligaments that normally hold the toe straight. It can be caused by the type of shoes you wear, your foot structure, trauma, and certain disease processes.
Symptoms
- Painful and/or difficult toe movement
- Swelling
- Joint stiffness
- Calluses/Corns
- Physical deformity
Risk Factors
- Age – The risk of hammertoe increases with age
- Sex – Women are more likely to have hammertoe compared to men
- Toe Length – You are more likely to develop hammertoe if your second toe is longer than your big toe
- Certain Diseases – Arthritis and diabetes may make you more likely to develop hammertoe
Treatment
If you have hammertoe, you should change into a more comfortable shoe that provides enough room for your toes. Exercises such as picking up marbles may strengthen and stretch your toe muscles. Nevertheless, it is important to seek assistance from a podiatrist in order to determine the severity of your hammertoe and see which treatment option will work best for you.
If you have any questions, please feel free to contact our office located in Chelan, WA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What Are Hammertoes?
Hammertoes are painful deformities that frequently form on the second, third, or fourth toe. The condition is often caused by an issue in foot mechanics. This can be caused by the person’s specific gait or the manner in which they walk, or by shoes that do not comfortably fit the deformity. Hammertoes can be formed after wearing shoes that are too narrow or short for the foot or have excessively high heels. Shoes that are not properly sized will force the toes into a bent position for long periods of time. This can cause the muscles to shorten and toes to bend into the deformity of a hammertoe.
Hammertoe can also be caused by complications from rheumatoid arthritis, osteoarthritis, trauma to the foot, heredity, or a cerebral vascular accident. Pain and difficult mobility of the toes, deformities, calluses, and corns are all symptoms of a hammertoe.
Someone who suspects they have the symptoms of a hammertoe should consult with a physician—particularly a podiatrist. Podiatrists diagnose and treat complications of the foot and ankle. If the podiatrist discovers that the affected toes are still flexible, treatment for the hammertoe may simply involve exercise, physical therapy, and better-fitting shoes. Treatment for hammertoes typically involves controlling foot mechanics, such as walking, through the use of customized orthotics.
For more serious cases in which the toes have become inflexible and rigid, surgery may be suggested. During the operation, the toe would receive an incision to relieve pressure on the tendons. A re-alignment of the tendons may then be performed by removing small pieces of bone to straighten the toe. In some cases, the insertion of pins is needed to keep the bones in the proper position as the toe heals. The patient is usually allowed to return home on the same day as the surgery.
If surgery is performed to repair a hammertoe, following the postoperative directions of your doctor is essential. Directions may include several stretches, picking up marbles with your toes, or attempting to crumple a towel placed flat against your feet. Wear shoes that have low heels and a wide amount of toe space to maintain comfort. Closed-toe shoes and high heels should be avoided. Shoes with laces allow the wearer to adjust how fitted he or she may want the shoes to be and also allow for greater comfort. To provide adequate space for your toes, select shoes that have a minimum of one-half inch of space between the tip of your longest toe and the inside of the shoe. This will also relieve pressure on your toes and prevent future hammertoes from forming.
Other preventative measures that can be taken include going shopping for new shoes in the middle of the day. Your feet are its smallest in the morning and swell as the day progresses. Trying on and purchasing new shoes midday will give you the most reliable size. Be sure to check that the shoes you purchase are both the same size. If possible, ask the store to stretch out the shoes at its painful points to allow for optimum comfort.
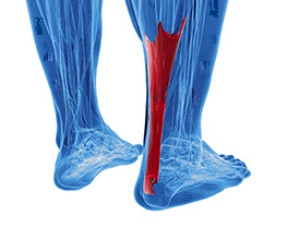
How the Achilles Tendon Can Be Injured
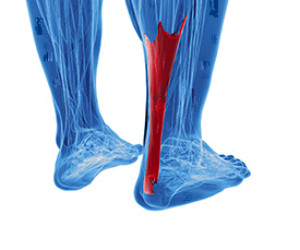 The Achilles tendon is located on the back of the ankle and connects the heel to the calf muscles. The two most common injuries that affect the Achilles tendon are Achilles tendinopathy and an Achilles tendon tear or rupture. Achilles tendinopathy symptoms include swelling, stiffness, and pain that is more noticeable in the morning. An Achilles tendon tear or rupture is often the result of forceful jumping and pivoting and sudden accelerations that result in overstretching and the eventual tearing of the tendon. A complete rupture can cause severe pain and a loss of strength and movement. Because of the seriousness of an Achilles tendon injury, patients who are experiencing pain and swelling in this tendon should consult with a podiatrist. A podiatrist will be able to help provide preventative measures to avoid a rupture, as well as guide you in healing the injury.
The Achilles tendon is located on the back of the ankle and connects the heel to the calf muscles. The two most common injuries that affect the Achilles tendon are Achilles tendinopathy and an Achilles tendon tear or rupture. Achilles tendinopathy symptoms include swelling, stiffness, and pain that is more noticeable in the morning. An Achilles tendon tear or rupture is often the result of forceful jumping and pivoting and sudden accelerations that result in overstretching and the eventual tearing of the tendon. A complete rupture can cause severe pain and a loss of strength and movement. Because of the seriousness of an Achilles tendon injury, patients who are experiencing pain and swelling in this tendon should consult with a podiatrist. A podiatrist will be able to help provide preventative measures to avoid a rupture, as well as guide you in healing the injury.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact John Horlebein, DPM of Northern Cascades Foot & Ankle, LLC. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our office located in Chelan, WA . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Achilles Tendon Injuries
The Achilles tendon is the largest tendon in the body; it is a tough band of fibrous tissue that stretches from the bones of the heel to the calf muscles. This tendon is what allows us to stand on our toes while running, walking, or jumping, it is common for this tendon to become injured. In severe cases, the Achilles tendon may become partially torn or completely ruptured. However, this tendon is susceptible to injury because of its limited blood supply and the high level of tension it endures.
The people who are more likely to suffer from Achilles tendon injuries are athletes who partake in activities that require them to speed up, slow down, or pivot. Consequently, athletes who engage in running, gymnastics, dance, football, baseball, basketball, or tennis are more likely to suffer from Achilles tendon injuries. Additionally, there are other factors that may make you more prone to this injury. People who wear high heels, have flat feet, tight leg muscles or tendons, or take medicines called glucocorticoids are more likely to have Achilles tendon injuries.
A common symptom of an Achilles tendon injury is pain above the heel that is felt when you stand on your toes. However, if the tendon is ruptured, the pain will be severe, and the area may become swollen and stiff. Other symptoms may be reduced strength in the lower ankle or leg area, and reduced range of motion in the ankle. When the Achilles tendon tears, there is usually a popping sound that occurs along with it. People who have acute tears or ruptures may find walking and standing to be difficult.
If you suspect you have injured your Achilles tendon, you should see your podiatrist to have a physical examination. Your podiatrist will likely conduct a series of tests to diagnose your injury including a “calf-squeeze” test. Calf squeeze tests are performed by first squeezing the calf muscle on the healthy leg. This will pull on the tendon and consequently cause the foot to move. Afterward, the same test will be performed on the injured leg. If the tendon is torn, the foot won’t move because the calf muscle won’t be connected to the foot.
HPV and Plantar Warts
Plantar warts are caused by the human papillomavirus (HPV). They occur on the sole of the feet—most typically on the balls of the feet, heels, and under the toes—and are spread by human contact when the virus enters the bloodstream through tiny cracks in the skin. They usually present as hard, thick, lesions akin to calluses, and sometimes tiny blood vessels are present, which look like black specks on the surface. Plantar warts can range in size, and are often tender or sometimes even painful. They can form as either independent growths or as part of a cluster of warts. While plantar warts can sometimes go away over a period of years, it is suggested that you seek the care of a podiatrist if you have circulatory problems or diabetes, or if your warts are painful, bleeding, or spreading quickly.
Plantar warts can be very uncomfortable. If you need your feet checked, contact John Horlebein, DPM from Northern Cascades Foot & Ankle, LLC. Our doctor will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our office located in Chelan, WA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.