September 2023
Effect of High Heels on the Feet
For hundreds of years, women have been wearing various kinds of high heels for aesthetic reasons. Women who wear high heels appear to be taller and have longer and thinner legs, and the wearer’s gait and posture changes. Though high heels have had an association with femininity and have kept them popular over the years, there are definite health problems caused by wearing them too frequently.
The motion of the ankle joints is limited when heels are worn. The ankle joint is very important to the body when it comes to walking. Because of their location, these joints have a great deal of weight put on them. Thus, it is very important to keep them as healthy as possible. The Achilles tendon is the main tendon in the ankle. Wearing high heels too often, studies have shown, can cause the calf muscle and Achilles tendon to shorten and stiffen. This can cause problems when shoes without heels are worn.
By putting a great deal of pressure on the ball of the foot and by forcing the toes into a small toe box, high heels can cause or may worsen many foot problems. These include corns, hammertoe, bunions, Morton’s neuroma and plantar fasciitis.
Not only does wearing high heels regularly have negative effects on the feet, the rest of the body can suffer as well. The knees, one of the most important joints in the entire body, can be affected by wearing high heels. High heels can cause the knees to stay bent all the time. Also, it can cause them to bend slightly inward as well. Doctors believe that women can suffer from osteoarthritis later in life because of constantly walking like in high heels. By limiting the natural motion of the foot during walking, high heels also cause an increased in stress on the knees.
Similarly, high heels can cause the back to go out of alignment. If high heels are worn constantly, the spine’s ability to absorb shock can cause continued back pain. They can compress the vertebrae of the lower back, and can overuse the back muscles.
However, this is not to say that high heels can never be worn. If worn occasionally and not often, they will not cause serious problems. They should not be worn every day. It’s important to wear them modestly to avoid the long-term physical health problems of the feet, knees, ankles, and back mentioned above.
How High Heels Can Affect the Feet

High heels have long been celebrated for their ability to elevate fashion and style. However, it is important to recognize that these fashionable footwear choices can come at a significant cost to the health of your feet. One of the primary concerns is the alteration of your foot's natural position. High heels force your body weight forward, causing an unnatural distribution of pressure. This can lead to conditions such as bunions, hammer toes, and metatarsalgia. Additionally, the increased pressure on the balls of your feet can cause pain and calluses. The elevated heels also reduce the length of your calf muscles, which can lead to shortening of the Achilles tendon and discomfort. Wearing high heels regularly may also contribute to balance issues and an increased risk of ankle sprains. While high heels may be a fashion statement, it is essential to wear them in moderation and prioritize your foot health. Consider lower-heeled options or flats for daily wear, saving those stylish stilettos for special occasions. If you would like more information about the dangers of wearing high heels, it is suggested that you confer with a podiatrist who can provide you with the knowledge you are seeking.
High heels have a history of causing foot and ankle problems. If you have any concerns about your feet or ankles, contact John Horlebein, DPM from Northern Cascades Foot & Ankle, LLC. Our doctor can provide the care you need to keep you pain-free and on your feet.
Effects of High Heels on the Feet
High heels are popular shoes among women because of their many styles and societal appeal. Despite this, high heels can still cause many health problems if worn too frequently.
Which Parts of My Body Will Be Affected by High Heels?
- Ankle Joints
- Achilles Tendon – May shorten and stiffen with prolonged wear
- Balls of the Feet
- Knees – Heels cause the knees to bend constantly, creating stress on them
- Back – They decrease the spine’s ability to absorb shock, which may lead to back pain. The vertebrae of the lower back may compress.
What Kinds of Foot Problems Can Develop from Wearing High Heels?
- Corns
- Calluses
- Hammertoe
- Bunions
- Morton’s Neuroma
- Plantar Fasciitis
How Can I Still Wear High Heels and Maintain Foot Health?
If you want to wear high heeled shoes, make sure that you are not wearing them every day, as this will help prevent long term physical problems. Try wearing thicker heels as opposed to stilettos to distribute weight more evenly across the feet. Always make sure you are wearing the proper shoes for the right occasion, such as sneakers for exercising. If you walk to work, try carrying your heels with you and changing into them once you arrive at work. Adding inserts to your heels can help cushion your feet and absorb shock. Full foot inserts or metatarsal pads are available.
If you have any questions please feel free to contact our office located in Chelan, WA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Limb Salvage
Limb salvage is a procedure that involves saving a lower extremity from amputation. In podiatry, limb amputation often occurs as a result of diabetes, peripheral vascular disease, neuropathy, cancer, and severe crush injury. The fundamental goal of limb salvage is to restore and maintain stability and movement of the affected lower extremity.
The procedure typically involves removing the diseased tissue and a small portion of the surrounding healthy tissue, as well as the removal of any affected bone if necessary. If the bone is removed, it is then replaced with prostheses, synthetic metal rods or plates, or grafts from either the patient’s body or a donor. Limb salvage is typically the preferred choice of procedure over amputation, as the procedure preserves both the patient’s appearance and allows for the greatest possible degree of function in the affected limb.
Upon diagnosis and determining that limb salvage is the appropriate treatment, the podiatrist may enlist the help of a physical and/or occupational therapist to prepare the patient for surgery by introducing various muscle-strengthening, walking, and range of motion exercises. Such exercises may be continued as rehabilitation post-procedure.
Possible Ways to Prevent Limb Loss

Losing a limb, particularly a lower extremity, is one of the greatest risks derived from diabetic foot ulcers. Preventing such a drastic outcome starts with undergoing an annual foot screening for those who have lost protective sensation in their feet. Next, experts believe that simple self-care techniques can allow patients to assume a certain amount of responsibility for their foot health. Knowledge of proper foot care and daily habits can go a long way in preserving limb health. This includes daily self-inspection. Regular and thorough self-examinations are critical for identifying early signs of foot injuries, calluses, or nail problems. By detecting issues such as blisters, redness, cracked skin, swelling, or abnormalities in their early stages, patients can prevent these problems from progressing into more severe conditions. Further, ill-fitting shoes that can make diabetic foot conditions worse include narrow-toed shoes, high heels, flip flops, or shoes that are too loose or tight. Timely intervention can help to prevent these issues from escalating into dire complications. If you are at risk for diabetic ulcers, it is suggested that you add a podiatrist to your medical team.
Limb salvage can be an effective way in preventing the need for limb amputation. If you have diabetes, cancer, or any other condition that could lead to foot amputation if left unchecked, consult with John Horlebein, DPM from Northern Cascades Foot & Ankle, LLC. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Limb Salvage?
Limb salvage is the attempt of saving a limb, such as the foot from amputation. Podiatrists also try to make sure that there is enough function in the foot after the salvage that it is still usable. Diabetes is the number one cause of non-traumatic amputations in the United States. Those with diabetes experience poor blood circulation, which prevents proper healing of an ulcer. If the ulcer is left uncheck, it could become infected, which could result in the need for amputation.
However, there are other causes as well, such as cancer and traumatic injury. Links between higher mortality rates and amputation have been found. This translates into higher healthcare costs, and a reduced quality of life and mobility for amputees. Podiatrists have attempted to increase the prevalence of limb salvage in an attempt to solve these issues.
Diagnosis and Treatment
Limb salvage teams have grown in recent years that utilize a number of different treatments to save the infected limb. This includes podiatrists that specialize in wound care, rehabilitation, orthotics, and surgery. Through a combination of these methods, limb salvage has been found to be an effective treatment for infected limbs, and as an alternative to amputation. Podiatrists will first evaluate the potential for limb salvage and determine if the limb can be saved or must be amputated.
If you have any questions, please feel free to contact our office located in Chelan, WA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
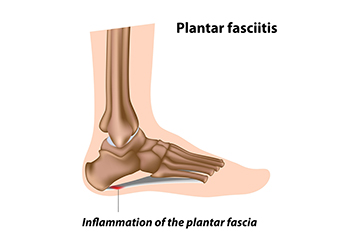
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
A Guide to Treating Plantar Fasciitis
Plantar fasciitis, a common and often debilitating foot condition, can bring your daily life to a halt due to severe heel pain. Fortunately, various treatment options are available to help you regain your comfort and mobility. Conservative measures like rest and taking anti-inflammatory medications can help to alleviate discomfort. Wearing supportive footwear with proper arch support and cushioning can significantly reduce strain on the plantar fascia. Stretching exercises that target the calf muscles and Achilles tendon can also provide relief by loosening tight structures around the foot. Custom orthotics may be recommended to support the arch and distribute pressure evenly. In rare cases, when conservative treatments are not sufficient, medical interventions such as cortico-steroid injections or surgery may be considered. Plantar fasciitis can be challenging, but with the right approach and patience, you can overcome it and return to a pain-free, active lifestyle. If you have heel pain, it is suggested that you contact a podiatrist who can effectively diagnose and treat plantar fasciitis.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact John Horlebein, DPM from Northern Cascades Foot & Ankle, LLC. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our office located in Chelan, WA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures are small breaks in the bone that are caused by repetitive stress. They typically occur due to overuse, forcing the bones of the foot or ankle to continually absorb the full impact of each step taken. Stress fractures can also be caused by abnormal foot structure, osteoporosis, bone deformities, or wearing improper footwear during exercise.
Stress fractures are common for individuals whose daily activities cause high levels of impact on their feet and ankles. Those who run, play tennis or basketball, or practice gymnastics tend to experience these fractures more frequently. Anyone is susceptible to this problem, though. Individuals who are normally sedentary and suddenly begin an intense, high impact workout may sustain stress fractures. This is because their muscles are not yet strong enough to handle and cushion the intensity of their activity. Osteoporosis may also cause someone to get stress fractures, because the disease weakens an afflicted person's bones and makes it easier for them to break down.
Pain from stress fractures typically occurs in the general area of the fracture. Pain can also manifest as “pinpoint pain” or pain that is felt when the site of the injury is touched, and can be accompanied by swelling. It may occur during or after activity, and it may disappear while resting and return when standing or moving. Engaging in any kind of activity, high impact or otherwise, will aggravate the pain. If the intensity of the activity increases before the stress fracture has properly healed, it can cause a full fracture.
Treatment can vary depending on the individual and the degree of injury. The primary way to treat a stress fracture is to rest the hurt foot. Some fractures will heal quickly with only a little bit of rest, while others may require a long rest period and the use of crutches, immobilization, or physical therapy. Under certain circumstances, surgery may be required to install support pins around the fracture to assist in healing.
If you are undergoing a new exercise regimen in running or some other kind of high impact activity, set incremental goals on a weekly basis so you can build up muscle strength. Make sure to wear supportive shoes to better protect you feet.
If you begin to experience any symptoms of stress fractures, you should stop exercising and rest. If the symptoms persist, consult with your podiatrist. Remembering these tips can help you prevent stress fractures to your foot and ankle, and allow you to continue living normally.
Causes and Risk Factors of Foot Stress Fractures

Stress fractures are microscopic cracks in bones, and can significantly impact foot health and mobility. These fractures are often the result of repetitive strain and overuse, which can gradually weaken the bones. Athletes, especially runners and dancers, are susceptible to developing a foot stress fracture, as a result of the constant impact on their feet. Sudden increases in activity intensity or duration can also trigger stress fractures. Factors such as wearing improper footwear, inadequate rest between activities, and poor foot structure can lead to a heightened risk of incurring a stress fracture. Additionally, medical conditions such as osteoporosis can reduce bone density, and increase vulnerability. Individuals with certain nutritional deficiencies, hormonal imbalances, or a history of stress fractures can face an elevated risk. Preventative measures include proper training progression, adequate nutrition, and wearing supportive shoes. If you have a foot stress fracture, it is suggested that you confer with a podiatrist who can effectively treat this condition.
Activities where too much pressure is put on the feet can cause stress fractures. To learn more, contact John Horlebein, DPM from Northern Cascades Foot & Ankle, LLC. Our doctor can provide the care you need to keep your pain free and on your feet.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures occur in the foot and ankle when muscles in these areas weaken from too much or too little use. The feet and ankles then lose support when walking or running from the impact of the ground. Since there is no protection, the bones receive the full impact of each step. Stress on the feet can cause cracks to form in the bones, thus creating stress fractures.
What Are Stress Fractures?
Stress fractures occur frequently in individuals whose daily activities cause great impact on the feet and ankles. Stress factors are most common among:
- Runners
- People affected with Osteoporosis
- Tennis or basketball players
- Gymnasts
- High impact workouts
Symptoms
Pain from the fractures occur in the area of the fractures and can be constant or intermittent. It will often cause sharp or dull pain with swelling and tenderness. Engaging in any kind of activity which involves high impact will aggravate pain.
If you have any questions please feel free to contact our office located in Chelan, WA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.